The Reproductive
System
|

uman reproduction,
always an object of the
most intense interest,
has lately become the
darling of the media,
the subject of
innumerable television
talk shows, magazine
articles, and newspaper
editorials. With each
new medical breakthrough
in fertility and family
planning, the noise
level grows higher. From
elementary school onward
we're now deluged with
information—some
factual, some not—on
menstruation and
menopause, conception
and contraception.
Sorting it all out may
seem impossible. But a
reasonable understanding
of the basics of
reproduction can make
the job easy. As you
weigh your options,
whether to encourage
pregnancy or forestall
it, your best resource
is a working knowledge
of the organs, glands,
and hormones that
prepare your body for
motherhood.
Our overview of the
reproductive system
begins at the external
genital area— or
vulva—which
runs from the pubic area
downward to the rectum.
Two folds of fatty,
fleshy tissue surround
the entrance to the
vagina and the
urinary opening: the
labia
majora, or outer
folds, and the
labia
minora, or inner
folds, located under the
labia majora. The
clitoris, is a
relatively short organ
(less than one inch
long), shielded by a
hood of flesh. When
stimulated sexually, the
clitoris can become
erect like a man's
penis. The
hymen,
a thin membrane
protecting the entrance
of the vagina, stretches
when you insert a tampon
or have intercourse.
From this point onward,
the reproductive system
leads deeper and deeper
into the body.
[return to top]
The vagina is a
muscular, ridged sheath
connecting the external
genitals to the uterus,
where the embryo grows
into a fetus during
pregnancy. In the
reproductive process,
the vagina functions as
a two-way street,
accepting the penis and
sperm during intercourse
and roughly nine months
later, serving as the
avenue of birth through
which the new baby
enters the world .
The vagina ends at the
cervix, the lower
portion or neck of the
uterus. Like the vagina,
the cervix has dual
reproductive functions.
After intercourse, sperm
ejaculated in the vagina
pass through the cervix,
then proceed through the
uterus to the
fallopian tubes
where, if a sperm
encounters an ovum
(egg), conception
occurs. The cervix is
lined with mucus, the
quality and quantity of
which is governed by
monthly fluctuations in
the levels of the two
principle sex hormones,
estrogen and
progesterone.
When estrogen levels are
low, the mucus tends to
be thick and sparse,
which makes it difficult
for sperm to reach the
fallopian tubes. But
when an egg is ready for
fertilization and
estrogen levels are high
the mucus then becomes
thin and slippery,
offering a much more
friendly environment to
sperm as they struggle
towards their goal.
(This phenomenon is
employed by
birth control pills,
shots and implants. One
of the ways they prevent
conception is to render
the cervical mucus
thick, sparse, and
hostile to sperm.)
|
|
HOW THE
SYSTEM FITS
TOGETHER
|
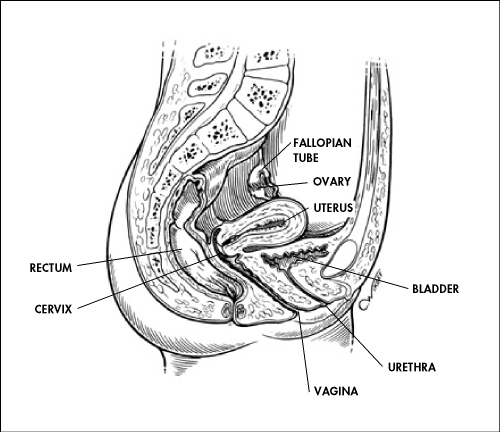
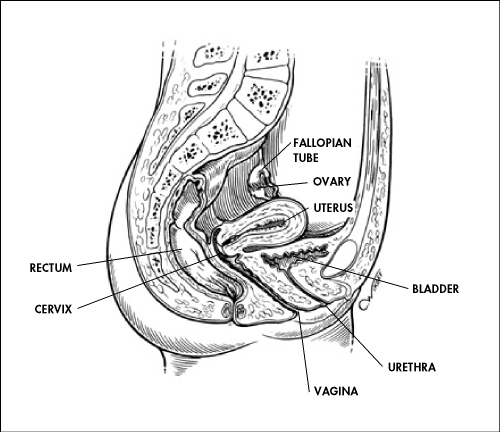
Deep within
the pelvic
region lie
the
specialized
female
organs that
make
conception
and
pregnancy
possible. In
this cutaway
view, you
can see how
the cervix
acts as the
gateway
between the
vagina and
the uterus,
where an
egg, if
fertilized,
will be
nurtured
and, over
the course
of nine
months, grow
to be a
newborn
child.
Riding atop
the uterus
are the two
ovaries,
storehouse
of all a
woman's
eggs. The
fallopian
tubes, where
fertilization
by a sperm
will occur,
are narrow
conduits
connecting
each ovary
to the
uterus.
|
|
|
Later, at the end of
pregnancy, the cervix
acts as the passage
through which the baby
exits the uterus into
the vagina. The cervical
canal expands to roughly
50 times its normal
width in order to
accommodate the passage
of the baby during
birth.
[return to top]
The uterus is the
muscular organ which
holds the developing
baby during the nine
months after conception.
Like the cervical canal,
the uterus expands
considerably during the
reproductive process. In
fact, the organ grows to
from 10 to 20 times its
normal size during
pregnancy.
|
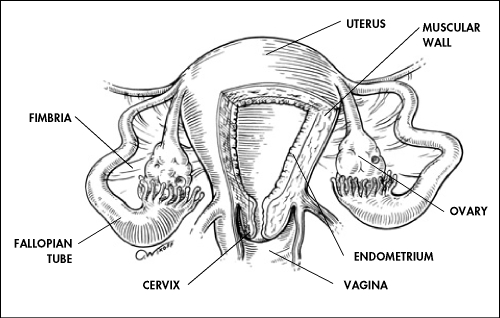
A CLOSER
LOOK AT THE
UTERUS
|
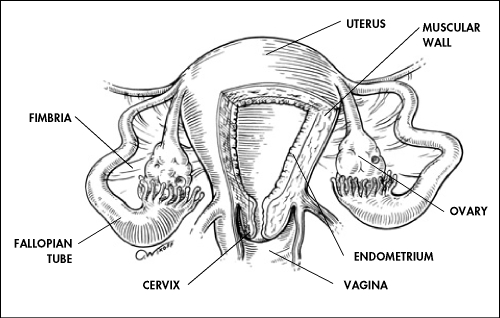
Note the
thick
muscular
walls—crucial
when the
baby is
ready for
delivery—and
the lush
inner
lining, or
endometrium,
which
nurtures the
developing
egg. From
this angle,
you can also
see how the
fallopian
tubes cradle
the ovaries
in their
feathery
fimbria,
ready to
conduct a
mature egg
away from
the ovary
and on into
the uterus.
|
Each month the uterus
goes through a cyclical
change, first building
up its endometrium or
inner lining to receive
a fertilized egg, then,
if conception does not
occur, shedding the
unused tissue through
the vagina in the
monthly process called
menstruation.
[return to top]
Beyond the uterus, the
fallopian tubes connect
the rest of the system
to the ultimate source
of the eggs, the two
ovaries. Each of these
tubes is roughly five
inches long and ranges
in width from about one
inch at the end next to
the ovary, to the
diameter of a strand of
thin spaghetti.
The trumpet-shaped part
near the ovary has about
20 to 25 feathery
projections called
fimbria, one of which is
attached to the ovary.
It is the fimbria that
each month urge an egg
to exit the ovary and
begin its trip towards
the uterus.
The ovaries are a
woman's storehouse of
egg cells. They are
among the first organs
to be formed as a female
baby develops in the
uterus. At the 20-week
mark, the structures
that will become the
ovaries house roughly 6
to 7 million potential
egg cells. From that
point on, the number
begins to decrease
rapidly. A newborn
infant has between 1
million to 2 million egg
cells. By puberty the
number has plummeted to
300,000. For every egg
that matures and
undergoes ovulation,
roughly a thousand will
fail, so that by
menopause, only a few
thousand remain. During
the course of an average
reproductive lifespan,
roughly 300 mature eggs
are produced for
potential conception.
The egg cells remain
inactive until puberty,
when the reproductive
system is activated by a
cascade of substances
called sex hormones.
Then, each month about
20 egg cells, each
encased in a sac called
a follicle, begin to
ripen. Responding
selectively to the sex
hormones, one follicle
becomes dominant while
the others shrink away.
The egg within the
dominant follicle
continues ripening to
maturity. Then, helped
by the feathery fimbria,
it exits the ovary and
enters the adjacent
fallopian tube to be
either fertilized or, if
conception fails to
occur, expelled from the
body during
menstruation.
If fertilization is to
occur, it usually
happens when the egg's
journey is about
one-third complete. Once
a sperm unites with the
egg, its surrounding
gelatinous coat releases
substances that prevent
more sperm from
entering.
[return to top]
The fertilized egg then
continues on its journey
through the fallopian
tube. About four or five
days after
fertilization, it enters
the uterus and implants
itself on the
endometrium, which has
been primed by the sex
hormones to accept and
nurture it.
|
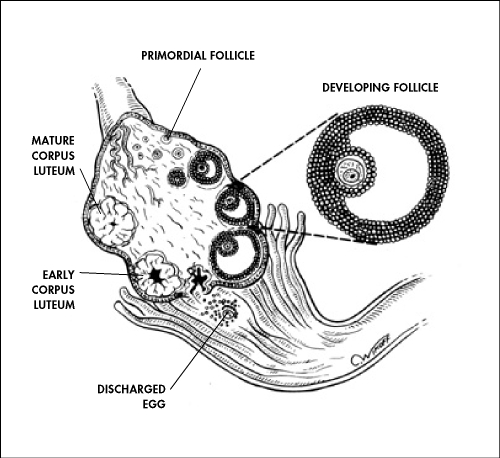
FROM
FOLLICLE TO
“YELLOW
BODY”
|
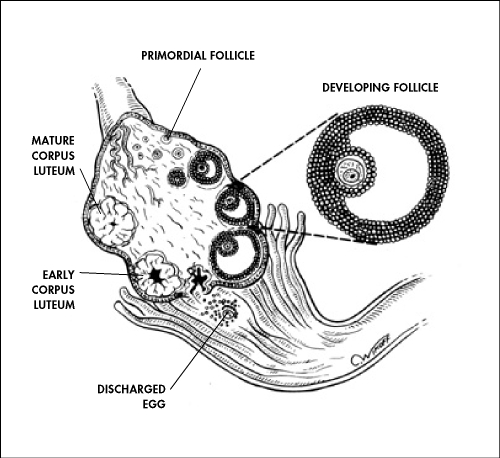
Host to a
lifetime
supply of
eggs, the
ovaries each
month launch
about 20
contenders
towards
potential
conception.
Each ripens
in a
supporting
follicle,
growth of
which is
triggered by
the aptly
named
“follicle-stimulating
hormone.” In
turn, the
winning
follicle
gives off
increasing
amounts of
the hormone
estrogen,
which
prepares the
lining of
the uterus
for
pregnancy.
Once a
mature egg
has begun
its trip
through the
fallopian
tube,
remnants of
the winning
follicle
form the
corpus
luteum, or
“yellow
body.”
Progesterone
from the
corpus
luteum halts
development
of the
remaining
follicles
and brings
the lining
of the
uterus to
peak
preparedness.
|
Meanwhile, the follicle
that held the egg still
has a critical role to
play. First it shrinks
markedly, then begins to
accumulate fatty
substances, or lipids,
that give it a yellowish
tinge. The resulting
structure, now called
the corpus luteum
(yellow body), produces
progesterone and
estradiol, two of the
hormones critical to
reproduction.
In a non-pregnant woman,
the corpus luteum lasts
for about 14 days, after
which it shrinks and
dries up, eventually
becoming a speck of
fibrous scar tissue. If
conception occurs,
however, a hormone from
the developing placenta,
which surrounds the baby
in the uterus,
stimulates the corpus
luteum to maintain its
production of
progesterone during the
first trimester of
pregnancy. |
|
|
|
| All living things reproduce. Reproduction — the process by which
organisms make more organisms like themselves — is one of the things
that sets living things apart from nonliving things. But even though the
reproductive system is essential to keeping a species alive, unlike
other body systems it's not essential to keeping an individual alive.
In the human reproductive process, two kinds of sex cells,
or gametes, are involved. The male gamete, or
sperm, and the female gamete, the egg or
ovum, meet in the female's reproductive system to
create a new individual. Both the male and
female reproductive systems are essential for reproduction.
Humans, like other organisms, pass certain characteristics of
themselves to the next generation through their genes,
the special carriers of human traits. The genes parents pass along to
their offspring are what make kids similar to others in their family,
but they're also what make each child unique. These genes come from the
father's sperm and the mother's egg, which are produced by the male and
female reproductive systems.
Understanding the male reproductive system, what it does, and the
problems that can affect it can help you better understand your son's
reproductive health.
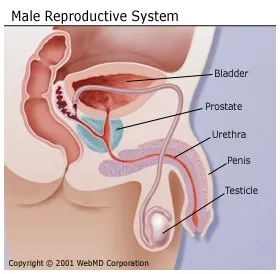
About the Male Reproductive System
Most species have two sexes: male and female. Each sex has its own
unique reproductive system. They are different in shape and structure,
but both are specifically designed to produce, nourish, and transport
either the egg or sperm.
Unlike the female, whose sex organs are located entirely within the
pelvis, the male has reproductive organs, or genitals,
that are both inside and outside the pelvis. The male genitals include:
- the testicles
- the duct system, which is made up of the epididymis and the vas
deferens
- the accessory glands, which include the seminal vesicles and
prostate gland
- the penis
In a guy who has reached sexual maturity, the two testicles,
or testes, produce and store millions of tiny sperm
cells. The testicles are oval-shaped and grow to be about 2 inches (5
centimeters) in length and 1 inch (3 centimeters) in diameter. The
testicles are also part of the endocrine system because they produce
hormones, including testosterone. Testosterone is a
major part of puberty in boys, and as a guy makes his way through
puberty, his testicles produce more and more of it. Testosterone is the
hormone that causes boys to develop deeper voices, bigger muscles, and
body and facial hair, and it also stimulates the production of sperm.
Alongside the testicles are the epididymis and the
vas deferens, which make up the duct system of the male
reproductive organs. The vas deferens is a muscular tube that passes
upward alongside the testicles and transports the sperm-containing fluid
called semen. The epididymis is a set of coiled tubes
(one for each testicle) that connects to the vas deferens.
The epididymis and the testicles hang in a pouch-like structure
outside the pelvis called the scrotum. This bag of skin
helps to regulate the temperature of testicles, which need to be kept
cooler than body temperature to produce sperm. The scrotum changes size
to maintain the right temperature. When the body is cold, the scrotum
shrinks and becomes tighter to hold in body heat. When it's warm, the
scrotum becomes larger and more floppy to get rid of extra heat. This
happens without a guy ever having to think about it. The brain and the
nervous system give the scrotum the cue to change size.
The accessory glands, including the seminal vesicles
and the prostate gland, provide fluids that lubricate the duct system
and nourish the sperm. The seminal vesicles are
sac-like structures attached to the vas deferens to the side of the
bladder. The prostate gland, which produces some of the
parts of semen, surrounds the ejaculatory ducts at the base of the
urethra, just below the bladder. The urethra is the
channel that carries the semen to the outside of the body through the
penis. The urethra is also part of the urinary system because it is also
the channel through which urine passes as it leaves the bladder and
exits the body.
The penis is actually made up of two parts: the
shaft and the glans. The shaft is the
main part of the penis and the glans is the tip (sometimes called the
head). At the end of the glans is a small slit or opening, which is
where semen and urine exit the body through the urethra. The inside of
the penis is made of a spongy tissue that can expand and contract.
All boys are born with a foreskin, a fold of skin at
the end of the penis covering the glans. Some boys are
circumcised, which means that a doctor or clergy member cuts
away the foreskin. Circumcision is usually performed during a baby boy's
first few days of life. Although circumcision is not medically
necessary, parents who choose to have their children circumcised often
do so based on religious beliefs, concerns about hygiene, or cultural or
social reasons. Boys who have circumcised penises and those who don't
are no different: All penises work and feel the same, regardless of
whether the foreskin has been removed.
What the Male Reproductive System Does
The male sex organs work together to produce and release semen into
the reproductive system of the female during sexual intercourse. The
male reproductive system also produces sex hormones, which help a boy
develop into a sexually mature man during
puberty.
When a baby boy is born, he has all the parts of his reproductive
system in place, but it isn't until puberty that he is able to
reproduce. When puberty begins, usually between the ages of 10 and 14,
the pituitary gland — which is located near the brain —
secretes hormones that stimulate the testicles to produce testosterone.
The production of testosterone brings about many physical changes.
Although the timing of these changes is different for every guy, the
stages of puberty generally follow a set sequence.
- During the first stage of male puberty, the scrotum and testes
grow larger.
- Next, the penis becomes longer, and the seminal vesicles and
prostate gland grow.
- Hair begins to appear in the pubic area and later it grows on
the face and underarms. During this time, a male's voice also
deepens.
- Boys also undergo a
growth spurt during puberty as they reach their adult height and
weight.
A male who has reached puberty will produce millions of sperm cells
every day. Each sperm is extremely small: only 1/600 of an inch (0.05
millimeters long). Sperm develop in the testicles within a system of
tiny tubes called the seminiferous tubules. At birth,
these tubules contain simple round cells, but during puberty,
testosterone and other hormones cause these cells to transform into
sperm cells. The cells divide and change until they have a head and
short tail, like tadpoles. The head contains genetic material (genes).
The sperm use their tails to push themselves into the epididymis, where
they complete their development. It takes sperm about 4 to 6 weeks to
travel through the epididymis.
The sperm then move to the vas deferens, or sperm duct. The seminal
vesicles and prostate gland produce a whitish fluid called
seminal fluid, which mixes with sperm to form semen when a male
is sexually stimulated. The penis, which usually hangs limp, becomes
hard when a male is sexually excited. Tissues in the penis fill with
blood and it becomes stiff and erect (an erection). The rigidity of the
erect penis makes it easier to insert into the female's vagina during
sexual intercourse. When the erect penis is stimulated, muscles around
the reproductive organs contract and force the semen through the duct
system and urethra. Semen is pushed out of the male's body through his
urethra — this process is called ejaculation. Each time
a guy ejaculates, it can contain up to 500 million sperm.
When the male ejaculates during intercourse, semen is deposited into
the female's vagina. From the vagina the sperm make their way up through
the cervix and move through the uterus with help from uterine
contractions. If a mature egg is in one of the female's fallopian tubes,
a single sperm may penetrate it, and fertilization, or
conception, occurs.
This fertilized egg is now called a zygote and
contains 46 chromosomes — half from the egg and half from the sperm. The
genetic material from the male and female has combined so that a new
individual can be created. The zygote divides again and again as it
grows in the female's uterus, maturing over the course of the pregnancy
into an embryo, a fetus, and finally a newborn baby.
Things That Can Go Wrong With the Male Reproductive System
Boys may sometimes experience reproductive system problems,
including:
Disorders of the Scrotum, Testicles, or Epididymis
Conditions affecting the scrotal contents may involve the testicles,
epididymis, or the scrotum itself.
- Testicular trauma. Even a mild injury to the
testicles can cause severe pain, bruising, or swelling. Most
testicular injuries occur when the testicles are struck, hit,
kicked, or crushed, usually during sports or due to other trauma.
Testicular torsion, when one of the testicles twists around, cutting
off its blood supply, is also a problem that some teen males
experience, although it's not common. Surgery is needed to untwist
the cord and save the testicle.
- Varicocele. This is a varicose vein (an
abnormally swollen vein) in the network of veins that run from the
testicles. Varicoceles commonly develop while a boy is going through
puberty. A varicocele is usually not harmful, although it can damage
the testicle or decrease sperm production. Take your son to see his
doctor if he is concerned about changes in his testicles.
- Testicular cancer. This is one of the most
common cancers in men younger than 40. It occurs when cells in the
testicle divide abnormally and form a tumor. Testicular cancer can
spread to other parts of the body, but if it's detected early, the
cure rate is excellent. Teen boys should be encouraged to learn to
perform testicular self-examinations.
- Epididymitis is inflammation of the epididymis,
the coiled tubes that connect the testes with the vas deferens. It
is usually caused by an infection, such as the sexually transmitted
disease chlamydia, and results in pain and swelling next to one of
the testicles.
- Hydrocele. A hydrocele occurs when fluid
collects in the membranes surrounding the testes. Hydroceles may
cause swelling in the scrotum around the testicle but are generally
painless. In some cases, surgery may be needed to correct the
condition.
- Inguinal
hernia. When a portion of the intestines pushes through
an abnormal opening or weakening of the abdominal wall and into the
groin or scrotum, it is known as an inguinal hernia. The hernia may
look like a bulge or swelling in the groin area. It can be corrected
with surgery.
Disorders of the Penis
Disorders affecting the penis include:
- Inflammation of the penis. Symptoms of penile
inflammation include redness, itching, swelling, and pain. Balanitis
occurs when the glans (the head of the penis) becomes inflamed.
Posthitis is foreskin inflammation, which is usually due to a yeast
or bacterial infection.
- Hypospadias. This is a disorder in which the
urethra opens on the underside of the penis, not at the tip.
- Phimosis. This is a tightness of the foreskin
of the penis and is common in newborns and young children. It
usually resolves itself without treatment. If it interferes with
urination, circumcision (removal of the foreskin) may be
recommended.
- Paraphimosis. This may develop when a boy's
uncircumcised penis is retracted but doesn't return to the
unretracted position. As a result, blood flow to the head of the
penis may be impaired, and your son may experience pain and
swelling. A doctor may use lubricant to make a small incision so the
foreskin can be pulled forward. If that doesn't work, circumcision
may be recommended.
- Ambiguous genitalia. This occurs when a child
is born with genitals that aren't clearly male or female. In most
boys born with this disorder, the penis may be very small or
nonexistent, but testicular tissue is present. In a small number of
cases, the child may have both testicular and ovarian tissue.
- Micropenis. This is a disorder in which the
penis, although normally formed, is well below the average size, as
determined by standard measurements.
If your son has symptoms of a problem with his reproductive system or
he has questions about growth and sexual development, talk with your
doctor — many problems with the male reproductive system can be treated.
|
The Male
Reproductive
System
The purpose of
the organs of
the male
reproductive
system is to
perform the
following
functions:
- To
produce,
maintain and
transport
sperm (the
male
reproductive
cells) and
protective
fluid
(semen)
- To
discharge
sperm within
the female
reproductive
tract during
sex
- To
produce and
secrete male
sex hormones
responsible
for
maintaining
the male
reproductive
system
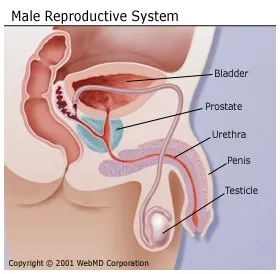
Unlike the
female
reproductive
system, most of
the male
reproductive
system is
located outside
of the body.
These external
structures
include the
penis, scrotum,
and testicles.
-
Penis:
This is the
male organ
used in
sexual
intercourse.
It has 3
parts: the
root, which
attaches to
the wall of
the abdomen;
the body, or
shaft; and
the glans,
which is the
cone-shaped
part at the
end of the
penis. The
glans, also
called the
head of the
penis, is
covered with
a loose
layer of
skin called
foreskin.
(This skin
is sometimes
removed in a
procedure
called
circumcision.)
The opening
of the
urethra, the
tube that
transports
semen and
urine, is at
the tip of
the penis.
The penis
also
contains a
number of
sensitive
nerve
endings.
The body of
the penis is
cylindrical
in shape and
consists of
3 circular
shaped
chambers.
These
chambers are
made up of
special,
sponge-like
tissue. This
tissue
contains
thousands of
large spaces
that fill
with blood
when the man
is sexually
aroused. As
the penis
fills with
blood, it
becomes
rigid and
erect, which
allows for
penetration
during
sexual
intercourse.
The skin of
the penis is
loose and
elastic to
accommodate
changes in
penis size
during an
erection.
Semen, which
contains
sperm
(reproductive
cells), is
expelled
(ejaculated)
through the
end of the
penis when
the man
reaches
sexual
climax
(orgasm).
When the
penis is
erect, the
flow of
urine is
blocked from
the urethra,
allowing
only semen
to be
ejaculated
at orgasm.
-
Scrotum:
This is the
loose
pouch-like
sac of skin
that hangs
behind the
penis. It
contains the
testicles
(also called
testes), as
well as many
nerves and
blood
vessels. The
scrotum acts
as a
"climate
control
system" for
the testes.
For normal
sperm
development,
the testes
must be at a
temperature
slightly
cooler than
body
temperature.
Special
muscles in
the wall of
the scrotum
allow it to
contract and
relax,
moving the
testicles
closer to
the body for
warmth or
farther away
from the
body to cool
the
temperature.
-
Testicles
(testes):
These are
oval organs
about the
size of
large olives
that lie in
the scrotum,
secured at
either end
by a
structure
called the
spermatic
cord. Most
men have two
testes. The
testes are
responsible
for making
testosterone,
the primary
male sex
hormone, and
for
generating
sperm.
Within the
testes are
coiled
masses of
tubes called
seminiferous
tubules.
These tubes
are
responsible
for
producing
sperm cells.
The Male
Reproductive
System
continued...
The internal
organs of the
male
reproductive
system, also
called accessory
organs, include
the following:
-
Epididymis:
The
epididymis
is a long,
coiled tube
that rests
on the
backside of
each
testicle. It
transports
and stores
sperm cells
that are
produced in
the testes.
It also is
the job of
the
epididymis
to bring the
sperm to
maturity,
since the
sperm that
emerge from
the testes
are immature
and
incapable of
fertilization.
During
sexual
arousal,
contractions
force the
sperm into
the vas
deferens.
- Vas
deferens:
The vas
deferens is
a long,
muscular
tube that
travels from
the
epididymis
into the
pelvic
cavity, to
just behind
the bladder.
The vas
deferens
transports
mature sperm
to the
urethra, the
tube that
carries
urine or
sperm to
outside of
the body, in
preparation
for
ejaculation.
-
Ejaculatory
ducts:
These are
formed by
the fusion
of the vas
deferens and
the seminal
vesicles
(see below).
The
ejaculatory
ducts empty
into the
urethra.
-
Urethra:
The urethra
is the tube
that carries
urine from
the bladder
to outside
of the body.
In males, it
has the
additional
function of
ejaculating
semen when
the man
reaches
orgasm. When
the penis is
erect during
sex, the
flow of
urine is
blocked from
the urethra,
allowing
only semen
to be
ejaculated
at orgasm.
-
Seminal
vesicles:
The seminal
vesicles are
sac-like
pouches that
attach to
the vas
deferens
near the
base of the
bladder. The
seminal
vesicles
produce a
sugar-rich
fluid
(fructose)
that
provides
sperm with a
source of
energy to
help them
move. The
fluid of the
seminal
vesicles
makes up
most of the
volume of a
man's
ejaculatory
fluid, or
ejaculate.
-
Prostate
gland:
The prostate
gland is a
walnut-sized
structure
that is
located
below the
urinary
bladder in
front of the
rectum. The
prostate
gland
contributes
additional
fluid to the
ejaculate.
Prostate
fluids also
help to
nourish the
sperm. The
urethra,
which
carries the
ejaculate to
be expelled
during
orgasm, runs
through the
center of
the prostate
gland.
-
Bulbourethral
glands:
Also called
Cowper's
glands,
these are
pea-sized
structures
located on
the sides of
the urethra
just below
the prostate
gland. These
glands
produce a
clear,
slippery
fluid that
empties
directly
into the
urethra.
This fluid
serves to
lubricate
the urethra
and to
neutralize
any acidity
that may be
present due
to residual
drops of
urine in the
urethra.
How Does the
Male
Reproductive
System Function?
The entire male
reproductive
system is
dependent on
hormones, which
are chemicals
that regulate
the activity of
many different
types of cells
or organs. The
primary hormones
involved in the
male
reproductive
system are
follicle-stimulating
hormone,
luteinizing
hormone, and
testosterone.
Follicle-stimulating
hormone is
necessary for
sperm production
(spermatogenesis)
and luteinizing
hormone
stimulates the
production of
testosterone,
which is also
needed to make
sperm.
Testosterone is
responsible for
the development
of male
characteristics,
including muscle
mass and
strength, fat
distribution,
bone mass,
facial hair
growth, voice
change and sex
drive.
|
|
The reproductive system includes the gonads -male testes and female
ovaries and other accessory ducts and glands (gonos = seed). These
provide the means for reproduction, the continuation of the species, and
passing on of genetic material to the next generation. Many of the
hormones associated with the reproductive system have already been
covered in the section about the
Endocrine
system. Puberty begins when hormones are secreted by the
pituitary glands, these control the growth and development of the
gonads.
Male reproductive organs include testes which produce spermatoza
and hormones; a series of ducts that store and transport the sperm;
accessory sex glands (including the prostate gland) secrete seminal
fluid, and the penis .
Female reproductive organs include the ovaries which produce
mature ova (eggs) and hormones; the fallopian tubes which transport ova
to the uterus; the vagina; the vulva; and also the mammary glands of the
breasts
Each breast has 15 to 20 sections called lobes, which have many smaller
sections called lobules. The lobes and lobules are connected by thin
tubes called ducts.
Development of the embryo. After successful fertilisation of the egg the
embryo is formed. At the end of the embryonic period (first two months)
the basis for all the main adult organs are present. This is followed by
the fetal period, during which the fetus develops.
Inheritance is the passing of hereditary traits from one
generation to the next - genetics .
| component
|
meaning
|
example
|
| ANTE- |
before
|
antenatal = before the birth of a baby
|
| COLP- |
vagina
|
e.g colpotomy = incision into the vaginal wall.
|
| MAMM-
|
breast
|
mammography = imaging of the breasts
|
| MAST- |
breast
|
mastectomy =surgical removal of a breast or part of a breast
|
| NEO-
|
new
|
neonatal = the first 4 weeks after birth
|
| GYN-
|
woman
|
gynocologist = medical specialist in diseases of the genital
tract in women.
|
- Breast Cancer Overview
- Breast cancer is the most common type of cancer in women aged
between 35 to 54, incidence has increased such that 1 in 9 women
develop breast cancer in the USA. Worldwide 700,000 cases are
diagnosed each year. The most common type of breast cancer that
found in the cells of the breast ducts, other types include those of
the lobes, and inflammatory breast cancer. If a lump is detected a
biopsy will be required to see if it malignant (most lumps are
benign). If the lump is cancerous hormone tests will be carried out
on the cells (estrogen and progesterone receptor tests). If the
cells are responsive to these hormones then these may be used to
stop the lump growing. Further treatment depends on the stage of the
cancer. Chemotherapy, surgery and radiotherapy may be required.
Total mastectomy is removal of the whole breast, in
radical mastectomy the chest muscles and under-arm lymph nodes
are also removed. More recently there has been an increased use of
lumpectomy where only the lump and surrounding tissue is
removed. Following surgery radiotherapy may be required.
Reconstructive surgery is the rebuilding the breast with other
tissue or implants, this may be done at the time of mastectomy or at
a later time. Between 5 and 10% of breast cancers are known to be
hereditary, women with the defective BRCA1 gene are more likely to
develop breast or ovarian cancer.
-
 Internet Resources for
Breast Cancer Internet Resources for
Breast Cancer
- Breast Cancer Prevention and Early Detection
- When breast cancer is found and treated early, a woman has more
treatment options and a better chance of cure. Both breast self
examination and screening programs have the potential to catch
breast cancer at a less advanced stage with a better chance of
survival.
- Male Breast Cancer
- Male breast cancer is uncommon, men account for approximately 1%
of all breast cancer cases. Incidence in Western populations is
under 1 case per 100,000 men, though rates reported in some African
countries are much higher. The majority of male breast cancers are
of the infiltrating ductal type, this is where the cancer has spread
beyond the cells lining ducts in the breast. In many respects male
breast cancer is similar to that found in women, though in general
men tend to be older than women at diagnosis. Treatment tends to be
the same as that for women with breast cancer of the same type and
stage.
-
 Internet Resources for Male
Breast Cancer Internet Resources for Male
Breast Cancer
- Gynacological (women's) Cancers
- Gynaecological cancers are a group of different malignancies of
the female reproductive system. The most common types of
gynaecologic malignancies are cervical cancer, ovarian cancer, and
endometrial (uterus) cancer. There are other less common
gynaecological malignancies including cancer of the vagina, cancer
of the vulva, gestational trophoblastic tumours, and fallopian tube
cancer. Occasionally skin cancers or sarcomas can also be found in
the female genitalia. Generally, most gynaecological cancers are
found in women aged over 50, though the incidence rates for younger
women have been rising.
-
 Internet Resources for
Gynaecological Cancers Internet Resources for
Gynaecological Cancers
- Cervical Cancer
- Cervical cancer is a common type of malignancy accounting for
about 6% of all cancers found in women. It is a disease in which
cancerous cells develop in the uterine cervix (this is the
connecting passage between the uterus and vagina). The peak
incidence of cervical cancer occurs between the ages of 40 to 55. It
is rare before the age of 35, however the incidence of cervical
cancer in younger women rose dramatically during the two decades
after 1960. Regular Pap smear tests may detect abnormal changes in
the cervical tissues, before cancer develops. Symptoms of cervical
cancer may include vaginal bleeding after intercourse or bleeding
between periods. However, in the early stages of the disease there
are often no obvious signs or symptoms, so regular smear tests are
important.
-
 Internet Resources for
Cervical Cancer Internet Resources for
Cervical Cancer
- Ovarian Cancer
- Cancer of the ovaries are the second most common group of
gynaecologic cancers, and account for about 5% of all women's
cancers. There are two main types; (i) epithelial tumours
(carcinomas) which account for 90% of ovarian cancers, and (ii)
non-epithelial tumours (eg. Stroma cell and germ cell tumours of the
ovary). The epithelial ovarian cancers are usually found in women
aged over 40, while the non-epithelial tumours are more common in
girls and young women. Epithelial ovarian cancer has few early
symptoms, a risk factor is having a family history of the disease.
Taking the contraceptive pill is known to be protective against
ovarian cancer.
-
 Internet Resources for
Ovarian Ca. Internet Resources for
Ovarian Ca.
- Vaginal Cancer
- Cancer of the vagina is relatively rare, accounting for about 2%
of gynaecological malignancies. There are two main types of vaginal
cancer; squamous cell cancer and adenocarcinoma. Over four fifths of
all vaginal cancers are squamous carcinoma, this is more common in
women between the ages of 60 and 80. The other type of vaginal
cancer; adenocarcinoma is usually found in young women under 30
years old.
-
 Internet Resources for
Vaginal Cancer Internet Resources for
Vaginal Cancer
- Uterus and Endometrial Carcinoma
- Endometrial cancer is a malignancy of the endometrium (the inner
lining of the uterus, or womb) and is the most common gynaecological
cancer, and accounts for 13% of all cancers in women. It is most
frequently in women over age 50. A know risk factor is prior
oestrogen-replacement therapy (however, oestrogen replacement also
lowers risk of heart disease). Symptoms can include pelvic pain, and
blood-soaked discharge - though these are also common symptoms
related to menopausal changes.
-
 Internet Resources for
Endometrial Ca. Internet Resources for
Endometrial Ca.
- Cancer of the Vulva
- The vulva is the outer part of the vagina, cancer of the vulvar
is a rare type of malignancy, usually found in women aged over 50 -
though the incidence of this cancer in younger women has been
reported to be increasing. Women with persistent itching and changes
in the colour vulva have a higher risk of cancer of the vulva.
Research suggests that human papillomavirus (HPV) may have a role in
causing this and other gynaecological cancers.
-
 Internet Resources for
Vulva Cancer Internet Resources for
Vulva Cancer
- Uterine Sarcoma
- Uterine sarcoma is a rare kind of cancer in which the cells in
the muscles or other supporting tissues of the uterus become
cancerous, and represents 1% of gynaecological cancers overall. This
is very different to endometrial (uterus) cancer - see above. There
are two main histological sub-types; leiomyosarcoma, and stromal
sarcoma. A known risk factor for developing uterine sarcoma is prior
radiotherapy to the pelvic area, this is estimated to account for
between 10% to 25% of cases.
-
 Internet Resources for
Uterine sarcoma Internet Resources for
Uterine sarcoma
- Gestational Trophoblastic Cancer
- Gestational trophoblastic tumour is a rare type of malignancy in
which the tissues formed in the uterus following conception become
cancerous. There are three types of gestational trophoblastic
tumours: (i) hydatidiform mole - this is where the sperm and egg
have joined but the tissues formed develop into a cyst; and (ii)
choriocarcinoma - this can begin from a hydatidiform mole or from
tissue that remains in the uterus following the delivery of a baby;
(iii) placental-site trophoblastic disease - this is very rare and
starts in the area of the uterus where the placenta was attached.
-
 Internet Resources for
Gestational Trophoblastic Disease Internet Resources for
Gestational Trophoblastic Disease
- Fallopian Tube Cancer
- Cancer starting in the fallopian tubes is very rare, less than
2,000 cases have been reported world-wide. Most cancers found in the
fallopian tubes have actually spread from other places such as the
ovaries. Most fallopian tube cancers are found in post menopausal
women.
-
 Internet Resources for
Fallopian Tube ca. Internet Resources for
Fallopian Tube ca.
- Genitourinary (Men's) Cancers
- The most common type of male genital malignancy is prostate
cancer (over 90% of male genital cancers), This is more common in
older men. Incidence rates have increased in recent years (SEER
data). Testicular cancer is less common (6% of male genital
cancers), but it is the most frequent cancer in young men between
the age of 15 to 35. Other types of cancers arising in the male
genitals are rare, these include penile cancer, scrotum cancers and
spermic cord cancer
-
 Internet Resources for
Genitourinary Cancers Internet Resources for
Genitourinary Cancers
- Testicular Cancer
- Testicular cancer is most common cancer in men between 15 to 35
years old. There are two broad types: seminoma and nonseminoma
histologies. The nonseminoma group of cancers includes embryonal
carcinoma, teratoma, yolk sac carcinoma and choriocarcinoma. The two
testicles (or testis) produce sperm and male hormones. Men who have
an undescended testicle (a testicle that didn't move down into the
scrotum) are at higher risk of developing testicular cancer.
World-wide about 36,000 men are diagnosed with testicular cancer
each year.
-
 Internet Resources for
Testicular Cancer Internet Resources for
Testicular Cancer
- Prostate Cancer
- Prostate cancer accounts for over a quater of all cancers in
men. The prostate is a small male sex gland located below the
bladder, it produces fluid that becomes semen. Prostate cancer
occurs mostly in older men, it is rare before the age of 50, and the
risk increases with age. There has been an increase in the incidence
of prostate cancer since the early 1980's, most likely due to an
increased use of screening using the prostate-specific antigen (PSA)
test. However, the role as screening for prostate cancer remains
controversial. World-wide about 395,000 men are diagnosed with
prostate cancer each year.
-
 Internet Resources for
Prostate Cancer Internet Resources for
Prostate Cancer
- Penile Cancer
- Cancer of the penis is rare in industrialised countries,
accounting for about 1% of male genital cancers, there are however
large international and racial differences in incidence. The disease
is more common in developing countries.
-
 Internet Resources for
Penile Cancer Internet Resources for
Penile Cancer
- Childhood Germcell Tumours
- Germ cell tumours (GCT) are most commonly found in children and
young adults. Germ cell tumours found in children tend to be of
different histology compared to those found in adults. Germ cells
are cells which become the embryo that develops in the womb. Some
germ cells may remain in different parts of the child's body after
birth and may give rise to tumours. The most common sites are the
testes, the ovaries or the sacrococcygael region. They may also
arise in other sites in the body e.g in the brain (intracranial
GCT). Germ Cell tumours produce alphafetoprotein (AFP) and human
chorionic gonadotrophin (HCG) that can be detected in blood samples
to aid diagnosis.
- Chemotherapy and Fertility
- Fertility may be affected by chemotherapy. Depending on the type
of drugs given there may be a risk of infertility. For female
patients certain drugs can cause permanent damage to the ovaries,
and the patient may have an early menopause. Male patients may also
be effected by chemotherapy which may cause a low sperm count. Male
patients who are old enough may leave a sample of sperm in a sperm
bank prior to chemotherapy.
Related Abbreviations and Acronyms:
-
-
| ABC |
Advanced Breast Cancer
|
| AFP |
Alphafetoprotein - eg. expressed by germ cell tumours
and other cancers
|
| BSE |
Breast Self Examination
|
| DCIS |
Ductal Carcinoma In Situ - type of breast cancer
|
| FIGO |
Federation Internat. Gyn. Obst. (FIGO Gynaecological
staging system)
|
| GCT |
Germ Cell Tumour
|
| GU |
Genito-urinary
|
| HPV |
Human Papilloma Virus - implicated in some gynacological
cancers
|
| HRT |
Hormone replacement therapy
|
| LCIS |
Lobular Carcinoma In Situ - type of breast cancer
|
| LMP |
Low Malignant Potential (context: ovarian tumours)
|
| Lx |
Lumpectomy
|
| Mx |
Mastectomy
|
| NABCO |
National Alliance of Breast Cancer Organizations
|
| PSA |
prostate-specific antigen - PSA test used in screening
for prostate cancer
|
| SGO |
Society of Gynecologic Oncologists
|
| YST |
Yolk sac tumour - (aka. germ cell tumour) |
 More Cancer Related
Abbreviations More Cancer Related
Abbreviations
|
 Internet Resources for
Breast Cancer
Internet Resources for
Breast Cancer