di·a·be·tes (di
 -be´t
-be´t z)
[ Gr. diab
z)
[ Gr. diab t
t s a
syphon, from dia through +bainein to go ]
s a
syphon, from dia through +bainein to go ]
1. any of various disorders characterized by
polyuria. 2.
d. mellitus.
adult-onset diabetes mellitus,
type 2 d.
mellitus.
alloxan diabetes, an animal model for diabetes mellitus;
administration of
alloxan produces selective destruction of the
beta cells of
the pancreas, causing hyperglycemia and ketoacidosis.
brittle diabetes,
type 1 diabetes
mellitus that is characterized by wide, unpredictable fluctuations
of blood glucose values and is difficult to control.
bronze diabetes, bronzed diabetes,
hemochromatosis.
central diabetes insipidus,
diabetes
insipidus due to injury of the neurohypophysial system, with a
deficient quantity of
vasopressin
being released or produced, causing failure of renal tubular
reabsorption of water. It may be inherited, acquired, or idiopathic.
Called also
pituitary d. insipidus.
chemical diabetes, former name for
impaired glucose
tolerance.
gestational diabetes, gestational diabetes mellitus,
diabetes mellitus
with onset or first recognition during pregnancy; it does not include
diabetics who become pregnant or women who become lactosuric.
growth-onset diabetes mellitus,
type 1 d.
mellitus.
diabetes insi´pidus, any of several types of
polyuria in
which the volume of urine exceeds 3 liters per day, causing dehydration
and great thirst, as well as sometimes emaciation and great hunger. The
underlying cause may be hormonal (central
d. insipidus) or renal (nephrogenic
d. insipidus).
insulin-dependent diabetes mellitus,
type 1 d.
mellitus.
juvenile diabetes mellitus, juvenile-onset diabetes mellitus,
type 1 d.
mellitus.
ketosis-prone diabetes mellitus,
type 1 d.
mellitus.
ketosis-resistant diabetes mellitus,
type 2 d.
mellitus.
latent diabetes, former name for
impaired glucose
tolerance.
lipoatrophic diabetes,
total
lipodystrophy.
malnutrition-related diabetes mellitus, a rare type of
diabetes mellitus
associated with chronic malnutrition and characterized by beta-cell
failure, insulinopenia, insulin resistance, and moderate to severe
hyperglycemia, but without ketosis. Called also
tropical or
tropical
pancreatic d. mellitus.
maturity-onset diabetes mellitus,
type 2 d.
mellitus.
maturity-onset diabetes of youth, maturity-onset diabetes of the
young, an autosomal dominant variety of
type 2 diabetes
mellitus, classified into several types on the basis of the mutation
involved, characterized by onset in late adolescence or early adulthood.
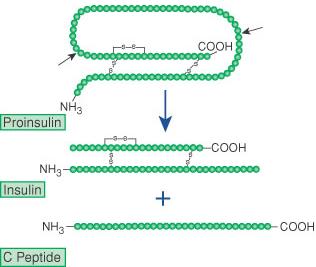
diabetes mel´litus, a chronic syndrome of impaired carbohydrate,
protein, and fat metabolism owing to insufficient secretion of insulin
or to target tissue insulin resistance. It occurs in two major forms:
type 1 d.
mellitus and
type 2 d. mellitus, which differ in etiology, pathology, genetics,
age of onset, and treatment.
nephrogenic diabetes insipidus,
diabetes
insipidus caused by failure of the renal tubules to reabsorb water
in response to
antidiuretic hormone, without disturbance in the renal filtration
and solute excretion rates; characterized by polyuria, extreme thirst,
growth retardation, and developmental delay. The condition does not
respond to exogenous vasopressin. It may be inherited as an X-linked
trait or be acquired as a result of drug therapy or systemic disease.
non–insulin-dependent diabetes mellitus,
type 2 d.
mellitus.
pituitary diabetes insipidus,
central d.
insipidus.
posttransplant diabetes, glucose intolerance or overt
hypoglycemia that first appears after an organ transplant; some cases
are steroid
diabetes caused by use of steroid
immunosuppressive
agents.
preclinical diabetes, former name for
impaired glucose
tolerance.
puncture diabetes, diabetes produced in an experimental animal by
puncturing the floor of the fourth ventricle in the medulla oblongata;
see Bernard
puncture, under puncture.
renal diabetes, see under
glycosuria.
steroid diabetes, steroidogenic diabetes, glucose intolerance or
overt hyperglycemia induced by glucocorticoids or estrogens; it is due
in part to target tissue insulin resistance and is characterized by a
relatively low incidence of microvascular sequelae.
subclinical diabetes, former name for
impaired glucose
tolerance.
thiazide diabetes, glucose intolerance or overt hyperglycemia
induced by
thiazide diuretics, which inhibit insulin secretion, possibly
through thiazide-induced
hypokalemia.
tropical diabetes mellitus, tropical pancreatic diabetes mellitus,
malnutrition-associated d. mellitus.
Type I diabetes mellitus,
type 1 d.
mellitus.
type 1 diabetes mellitus, one of the two major types of diabetes
mellitus, characterized by abrupt onset of symptoms,
insulinopenia,
and dependence on exogenous
insulin to
sustain life; peak age of onset is 12 years, although onset can be at
any age. It is due to lack of insulin production by the
beta cells of
the pancreas, which may result from viral infection,
autoimmune
reactions, and probably genetic factors;
islet cell
antibodies are usually detectable at diagnosis. When it is inadequately
controlled, lack of insulin causes
hyperglycemia,
protein wasting,
and production of
ketone bodies owing to increased fat metabolism, and the
hyperglycemia
leads to overflow
glycosuria, osmotic
diuresis,
hyperosmolarity,
dehydration,
and diabetic
ketoacidosis. It is accompanied by
angiopathy of
blood vessels, particularly the small ones (microangiopathy),
which affects the retinas, kidneys, and basement membrane of arterioles
throughout the body. Other symptoms include
polyuria,
polydipsia,
polyphagia,
weight loss,
paresthesias, blurred vision, and irritability; if untreated,
diabetic
ketoacidosis progresses to nausea and vomiting, stupor, and
potentially fatal hyperosmolar coma (diabetic
coma). Called also
insulin-dependent,
juvenile,
juvenile-onset,
and Type I d.
mellitus.
Type II diabetes mellitus,
type 2 d.
mellitus.
type 2 diabetes mellitus, one of the two major types of diabetes
mellitus, characterized by peak age of onset between 50 and 60 years,
gradual onset with few symptoms of metabolic disturbance (glycosuria
and its consequences), and no need for exogenous
insulin;
dietary control with or without oral
hypoglycemic
is usually effective.
Obesity and
genetic factors may also be present. Diagnosis is based on laboratory
tests indicating
glucose intolerance. Basal
insulin
secretion is maintained at normal or reduced levels, but insulin release
in response to a
glucose load is delayed or reduced. Defective glucose receptors on
the beta cells
of the pancreas may be involved. It is often accompanied by disease of
various sizes of blood vessels, particularly the large ones, which leads
to premature
atherosclerosis with
myocardial
infarction or
stroke syndrome. Called also
adult-onset,
maturity-onset,
non–insulin-dependent, and
Type II d.
mellitus.

 -be´t
-be´t z)
[ Gr. diab
z)
[ Gr. diab
 Diabetes
is a disorder characterized by hyperglycemia or elevated blood
glucose (blood sugar). Our bodies function best at a certain
level of sugar in the bloodstream. If the amount of sugar in our
blood runs too high or too low, then we typically feel bad.
Diabetes is the name of the condition where the blood
sugar level consistently runs too high. Diabetes is the
most common endocrine disorder. Sixteen million Americans have
diabetes, yet many are not aware of it. African Americans,
Hispanics and Native Americans have a higher rate of developing
diabetes during their lifetime. Diabetes has potential long term
complications that can affect the kidneys, eyes, heart, blood
vessels and nerves. A number of pages on this web site are
devoted to the prevention and treatment of the complications of
diabetes.
Diabetes
is a disorder characterized by hyperglycemia or elevated blood
glucose (blood sugar). Our bodies function best at a certain
level of sugar in the bloodstream. If the amount of sugar in our
blood runs too high or too low, then we typically feel bad.
Diabetes is the name of the condition where the blood
sugar level consistently runs too high. Diabetes is the
most common endocrine disorder. Sixteen million Americans have
diabetes, yet many are not aware of it. African Americans,
Hispanics and Native Americans have a higher rate of developing
diabetes during their lifetime. Diabetes has potential long term
complications that can affect the kidneys, eyes, heart, blood
vessels and nerves. A number of pages on this web site are
devoted to the prevention and treatment of the complications of
diabetes.  The
human body wants blood glucose (blood sugar) maintained in a
very narrow range. Insulin and glucagon are the hormones which
make this happen. Both insulin and glucagon are secreted from
the pancreas, and thus are referred to as pancreatic endocrine
hormones. The picture on the left shows the intimate
relationship both insulin and glucagon have to each other. Note
that the pancreas serves as the central player in this scheme.
It is the production of insulin and glucagon by the pancreas
which ultimately determines if a patient has diabetes,
hypoglycemia, or some other sugar problem.
The
human body wants blood glucose (blood sugar) maintained in a
very narrow range. Insulin and glucagon are the hormones which
make this happen. Both insulin and glucagon are secreted from
the pancreas, and thus are referred to as pancreatic endocrine
hormones. The picture on the left shows the intimate
relationship both insulin and glucagon have to each other. Note
that the pancreas serves as the central player in this scheme.
It is the production of insulin and glucagon by the pancreas
which ultimately determines if a patient has diabetes,
hypoglycemia, or some other sugar problem.