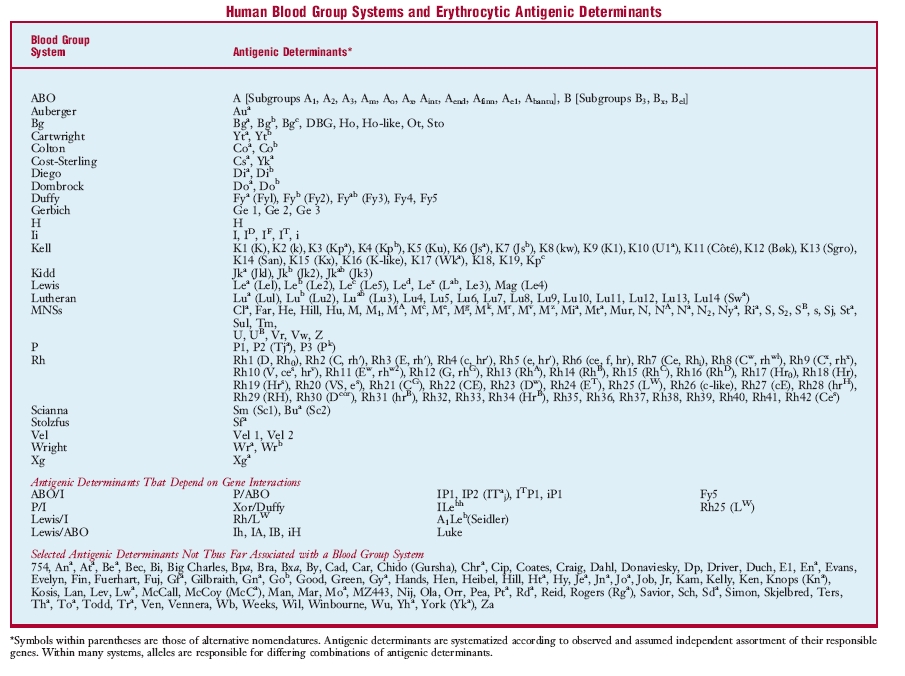
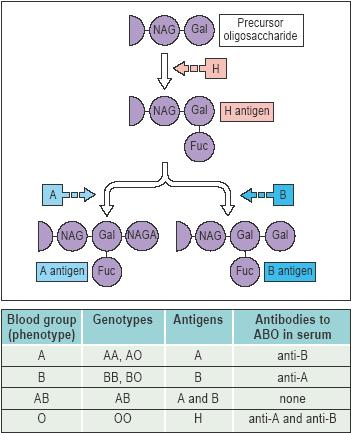
| ABO blood group, the major human blood group system, dependent on the presence or absence of A and B antigens, which are largely glycolipids on the cell membrane. The gene for A is responsible for synthesis of N-acetyl-α-d-galactosaminyl transferase, whereas that for B is responsible for α-d-galactosyl transferase. Either A or B is created when one of these hexasaccharides is positioned by a specific transferase in 1→3 linkage to the β-d-galactose of an H-active oligosaccharide. Type O occurs when neither transferase is present or, very rarely (Bombay phenotype), when H antigen does not exist. When both transferases are present, type AB results. Differences in degree of transferase activity are determined at the same locus: weak transferase gives rise to weak antigens (A2, A3Ax, B3Bx). Similar oligosaccharides, especially in bacterial cell walls, immunize persons lacking A or B so that their serum contains anti-A or anti-B activity. A and B antigens are on the mucopolysaccharides of secretors; persons with dominant genes have H-active mucoids. |
| Auberger blood group, a blood group consisting of the erythrocytic antigen Aua, related to the Lutheran blood group. |
| Bg blood group, a blood group consisting of the erythrocytic human leukocyte antigens Bga, Bgb, Bgc, DBG, Ho, Ho-like, Ot, and Sto. |
| Cartwright blood group, Yt b. g. |
| Chido-Rodgers blood group, a blood group consisting of antigens Cha and Rga, antigenic determinants of fragments of the C4 component of complement. |
| Colton blood group, a blood group consisting of erythrocytic antigens Coa and Cob. |
| Cromer blood group, a blood group consisting of erythrocytic antigens Cra, Tca, Tcab, Dra, Esa, WESb, UMC, and IFC, which are located on the membrane protein called decay accelerating factor. |
| Diego blood group, a blood group consisting of the erythrocytic antigens Dia and Dib, determined by allelic genes. Dia is most frequent in South American Indians, Japanese, and Chinese. |
| Dombrock blood group, a blood group consisting of the erythrocytic antigens Doa and Dob, most common in people of European descent. |
| Duffy blood group, a blood group consisting principally of the erythrocytic antigens Fya and Fyb, determined by allelic genes. Amorphic genes are common in individuals of African descent. |
| Gerbich blood group, a blood group consisting of the erythrocytic antigens Ge 1, Ge 2, and Ge 3; although rare in most parts of the world, it has been found often in Papua New Guinea. |
| H blood group, a blood group consisting of antigen H; see also Bombay phenotype. |
| high frequency blood group, a group containing over 99 per cent of individuals, who have a type of erythrocyte antigens called public antigens. |
| Ii blood group, a high frequency blood group involving receptors of most cold reactive hemagglutinins; it is expressed most strongly on cord blood cells. |
| Kell blood group, a blood group consisting of multiple erythrocytic antigens, especially three pairs of alternates, determined by complex genes at one locus, including an amorph; also regulated by the X chromosome, it is associated with sex-linked chronic granulomatous disease. One antigen, K6, is more frequent in people of African descent. |
| Kidd blood group, a blood group consisting principally of Jka and Jkb antigens, determined by allelic genes; amorphic genes are most common in those of East Asian descent. |
| Knops blood group, a blood group consisting of antigens Kna, Knb, McCa, Sla, and Yka, which are located on complement receptor type 1. |
| Lan blood group, a blood group consisting of the erythrocytic antigen Lan. |
| Lewis blood group, a blood group determined by plasma glycolipids that adhere to erythrocytic surfaces. It is based on dominant independent Le genes, but interacts with the H precursor oligosaccharides of A and B. Whereas le/le provides the “double negative” blood type Le(a−b−), Le without H gives rise to Lea, i.e., blood type Le(a+b−), and that with H gives rise to LebH, i.e., blood type Le(a−b+). |
| low frequency blood group, any small group that has erythrocytic antigens found in fewer than 1 per cent of the population (private antigens). |
| Lutheran blood group, a complex blood group system consisting of antigens Lua and Lub; it somewhat resembles the Kell group in having pairs of alternative antigens and amorphic genes, but is also subject to a dominant independently segregating repressor. |
| MNSs blood group, a complex blood group system consisting principally of two pairs of antigens determined by closely linked genes (crossovers have been observed, but rarely). M and N, determined by allelic genes, depend on sialic (neuraminic) acid residues. S and s are also determined by allelic genes, and an amorphic gene is common in blacks when another antigen (U) is missing. The system also includes numerous low frequency antigens. |
| P blood group, a blood group system originally consisting of only P (now P1) antigen, but later found to include P2 (Tja), a very high frequency antigen, and P3 (PK), a very low frequency antigen. P1 is most common in people of African descent (90 per cent), less so in those of European descent (75 per cent), and least in those of East Asian descent (30 per cent). |
| Rh blood group, the most complex of all human blood groups because the genes differ by determining different numbers of antigens (Rh factors) and do so with remarkably different quality; over 40 antigens have been described to date. People of African descent show the greatest degree of diversity and East Asians the least. The major antigen, Rh1 (Rh0, D, or Rh0D), is highly immunogenic and before the development of passive immunization prophylaxis it was responsible for serious hemolytic disease of the newborn. Two other pairs of alternative antigens are inherited with or without Rh1; these are Rh21 (rhG or CG) and Rh4 (hr´ or c), and Rh3 (rh´ or E) and Rh5 (hr´ or e). The most common groups of antigens are R−1,−3,−21 (in Caucasians), R1,−3,−21 (in blacks), R1,−3,21 (in East Asians and Caucasians), and R1,3,−21 (in East Asians and Caucasians). Another antigen Rh10 (hrv, V) is common in blacks. |
| Scianna blood group, a blood group consisting of erythrocytic antigens Sc1 (formerly Sm) and Sc2 (formerly Bua). |
| Sid blood group, a blood group consisting of those with extra amounts of the public erythrocytic antigen Sda, referred to as Sd(a++). |
| Vel blood group, a blood group consisting of the erythrocytic antigens Vel 1 and Vel 2. |
| Wright blood group, a blood group consisting of the erythrocytic antigens Wra and Wrb. |
| Xg blood group, a blood group consisting of erythrocytic antigen Xga, which is determined by a gene on the long arm of the X chromosome. |
| Yt blood group, a blood group consisting of the erythrocytic antigens Yta and Ytb. Called also Cartwright b. g. |
| blood pressure, the pressure of blood against the walls of any blood vessel.the pressure of the blood on the walls of the arteries, dependent on the energy of the heart action, the elasticity of the walls of the arteries, and the volume and viscosity of the blood. The maximum or systolic blood pressure occurs near the end of the stroke output of the left ventricle of the heart. The minimum or diastolic blood pressure occurs late in ventricular diastole. Mean blood pressure is the average of the blood pressure levels, and basic blood pressure is that during quiet rest or basal conditions. See also hypertension and hypotension. |
| reported in mmHg or mm Hemoglobin, |
| diastole |
| the dilatation, or period of dilatation, of the heart, especially of the ventricles; it coincides with the interval between the second and the first heart sounds. Cf. systole and see illustration at cardiac cycle, under cycle. |
| electrical diastole, that time during which the cell rests; it is represented by phase 4 of the action potential. |
| output |
| the yield; the total of anything produced by any functional system of the body. |
| basal acid output, on the pentagastrin test, the output of gastric acid for one hour with minimal stimulation in a fasting patient, expressed as mmol/hr. |
| cardiac output, the effective volume of blood expelled by either ventricle of the heart per unit of time (usually volume per minute); it is equal to the stroke volume multiplied by the heart rate. |
| energy output, the energy a body is able to manifest in work or activity. |
| maximal acid output, on the pentagastrin test, the output of gastric acid for one hour after administration of pentagastrin, expressed as mmol/hr. |
| peak acid output, on the pentagastrin test, after administration of pentagastrin, the sum of the two highest 15-minute outputs of gastric acid multiplied by 2, expressed as mmol/hr. |
| stroke output, see under volume. |
| urinary output, the amount of urine excreted by the kidneys. |
| work output of the heart, the amount of energy that the heart converts to work; usually expressed per heart beat (stroke work o.) or per minute (minute work o.). |
| hypotension |
| abnormally low blood pressure; seen in shock but not necessarily indicative of it. |
| chronic idiopathic orthostatic hypotension, chronic orthostatic hypotension, idiopathic orthostatic hypotension, Shy-Drager syndrome.Bradbury-Eggleston syndrome. |
| intradialytic hypotension, hypotension sometimes seen as a complication of hemodialysis. |
| orthostatic hypotension, postural hypotension, a fall in blood pressure associated with dizziness, blurred vision, and sometimes syncope, occurring upon standing or when standing motionless in a fixed position; it can be acquired or idiopathic, transient or chronic, and may occur alone or secondary to a disorder of the central nervous system such as the Shy-Drager syndrome. |
| supine hypotension, see under syndrome. |
| vascular hypotension, severe hypotension from dilatation of the blood vessels. |
| hypertension |
| high arterial blood pressure; various criteria for its threshold have been suggested, ranging from 140 mm Hg systolic and 90 mm Hg diastolic to as high as 200 mm Hg systolic and 110 mm Hg diastolic. Hypertension may have no known cause (essential or idiopathic h.) or be associated with other primary diseases (secondary h.). |
| accelerated hypertension, progressive hypertension marked by the funduscopic vascular changes of malignant hypertension but without papilledema. |
| adrenal hypertension, hypertension caused by an adrenal tumor that secretes mineralocorticoids, such as in hyperaldosteronism; in many cases it may be associated with excessive production of other adrenocortical hormones normally made in minute amounts. |
| benign intracranial hypertension, pseudotumor cerebri. |
| borderline hypertension, a condition in which the arterial blood pressure is sometimes within the normotensive range and sometimes within the hypertensive range; called also labile h. |
| chronic thromboembolic pulmonary hypertension, persistent pulmonary hypertension due to obstruction of a major pulmonary artery by an unresolved embolus. |
| essential hypertension, hypertension occurring without discoverable organic cause; called also primary h. and idiopathic h. |
| familial dyslipidemic hypertension, an inherited syndrome of seriously disordered blood lipid levels and essential hypertension. |
| gestational hypertension, pregnancy-induced h. |
| Goldblatt hypertension, hypertension experimentally induced with clamping that causes a Goldblatt kidney; called also Goldblatt phenomenon. |
| idiopathic hypertension, essential h. |
| idiopathic intracranial hypertension, pseudotumor cerebri. |
| intracranial hypertension, increased intracranial pressure; if symmetrically distributed it may have few neurologic symptoms (see pseudotumor cerebri), but if it is asymmetrical, as with hydrocephalus, neurologic symptoms are often severe. |
| labile hypertension, borderline h. |
| low-renin hypertension, essential hypertension associated with low levels of plasma renin concentration or low renin activity. |
| malignant hypertension, a severe hypertensive state with poor prognosis; it is characterized by papilledema of the ocular fundus with vascular exudative and hemorrhagic lesions, medial thickening of small arteries and arterioles, and left ventricular hypertrophy. Diastolic pressures as high as 130 mm Hg or more are commonly present. |
| ocular hypertension, persistently elevated intraocular pressure in the absence of any other signs of glaucoma; it may or may not progress to open-angle glaucoma. |
| persistent pulmonary hypertension of the newborn, a condition in newborns in which blood continues to flow through the foramen ovale and a patent ductus arteriosus, bypassing the lungs and resulting in hypoxemia. Called also persistent fetal circulation. |
| portal hypertension, abnormally increased blood pressure in the portal venous system, a frequent complication of cirrhosis. |
| hypertension of pregnancy, pregnancy-induced hypertension, the spectrum of preeclampsia and eclampsia. |
| primary hypertension, essential h. |
| pulmonary hypertension, pulmonary arterial hypertension, increased pressure (above 30 mm Hg systolic and 12 mm Hg diastolic) within the pulmonary arterial circulation. |
| renal hypertension, hypertension due to or associated with renal disease with a factor of parenchymal ischemia. |
| renovascular hypertension, hypertension due to occlusive disease of the renal arteries such as renal artery stenosis or fibromuscular dysplasia. |
| secondary hypertension, hypertension due to or associated with a variety of primary diseases, such as renal disorders, disorders of the central nervous system, endocrine diseases, and vascular diseases. |
| splenoportal hypertension, obstruction of the splenic venous system resulting in enlargement of the liver and manifestation of ascites and other evidence of portal cirrhosis. |
| symptomatic hypertension, hypertension accompanied by symptoms such as dizziness or headache. |
| systemic venous hypertension, elevation of systemic venous pressure, usually detected by inspection of the jugular veins. |
| vascular hypertension, hypertension. |